Telehealth Platform Comparison 2025: US Practice Guide

This article provides a comprehensive telehealth platform comparison for US practices in 2025, meticulously analyzing features, costs, integration capabilities, and financial implications to guide informed decision-making for optimal patient care and operational efficiency.
The landscape of healthcare delivery is rapidly evolving, with telehealth firmly established as a cornerstone of modern medical practice. For US healthcare providers, selecting the right telehealth platform comparison in 2025 is no longer a luxury but a strategic imperative, demanding a deep dive into features, costs, integration capabilities, and the profound financial impact on their operations and patient care.
Understanding the Telehealth Evolution in 2025
Telehealth has transcended its initial role as an emergency response during the pandemic, solidifying its position as an integral part of the US healthcare system. As we move into 2025, the market for telehealth platforms is more mature, sophisticated, and competitive than ever before. Practices are seeking solutions that not only facilitate virtual visits but also enhance patient engagement, streamline administrative tasks, and comply with evolving regulatory frameworks.
The shift towards value-based care models and the increasing demand for convenient, accessible healthcare have fueled innovation in telehealth. Providers must navigate a complex ecosystem of vendors, each offering a unique blend of functionalities. A thorough understanding of these offerings is crucial to making an informed decision that aligns with both clinical needs and business objectives.
Regulatory Landscape and Compliance
The regulatory environment for telehealth in the US continues to evolve, with significant implications for platform selection. Adherence to HIPAA, state-specific licensing requirements, and reimbursement policies are paramount.
- HIPAA Compliance: Ensures patient data privacy and security, a non-negotiable feature for any telehealth platform.
- State-Specific Regulations: Varies by state, impacting cross-state practice and prescribing capabilities.
- Reimbursement Policies: Understanding current and projected Medicare, Medicaid, and private payer reimbursement rules is vital for financial viability.
Choosing a platform that proactively addresses these regulatory complexities can save practices significant headaches and potential penalties. It’s not enough for a platform to simply offer virtual visits; it must do so within a robust, compliant framework.
The continuous evolution of telehealth necessitates ongoing evaluation of platforms to ensure they remain compliant and effective. Practices must look beyond immediate needs and consider how a platform can adapt to future regulatory changes and technological advancements, securing their investment for the long term.
Key Features to Evaluate in Telehealth Platforms
When undertaking a telehealth platform comparison, a meticulous examination of core features is essential. Beyond basic video conferencing, modern platforms offer a suite of tools designed to optimize patient care and practice efficiency. These features can significantly impact patient satisfaction, clinician workflow, and overall operational success.
The ideal telehealth solution should act as an extension of the physical clinic, providing a seamless and secure environment for virtual interactions. This includes capabilities that support the entire patient journey, from initial scheduling to post-visit follow-up, ensuring continuity of care.
Core Functionality and User Experience
A user-friendly interface for both patients and providers is paramount. If a platform is difficult to navigate, adoption rates will suffer, undermining the investment. Providers need intuitive tools for managing appointments, conducting calls, and accessing patient information efficiently.
- High-Quality Video/Audio: Essential for clear communication and effective virtual examinations.
- Secure Messaging: Enables HIPAA-compliant asynchronous communication between patients and providers.
- Virtual Waiting Room: Manages patient flow and provides a professional, organized start to virtual appointments.
- Screen Sharing & Document Exchange: Facilitates sharing of educational materials, lab results, and other relevant documents.
Beyond these basics, consider features like multi-party calling for family involvement, virtual background options for privacy, and robust technical support. A platform that prioritizes user experience ultimately enhances both patient and provider satisfaction, fostering a more positive telehealth environment.
Evaluating the core functionalities against the specific needs of your practice is crucial. A specialist might require different tools than a general practitioner, emphasizing the need for a tailored approach to platform selection. The goal is to find a platform that enhances, rather than complicates, clinical workflows.
Cost Analysis: Unpacking Telehealth Platform Pricing Models
The financial implications of adopting a telehealth platform are a major consideration for any US practice. A comprehensive telehealth platform comparison must delve into the various pricing models and hidden costs to ensure a sustainable investment. Understanding where your money goes is key to avoiding unexpected expenses and maximizing ROI.
Telehealth platform costs can vary widely based on features, user count, and support levels. Practices should look beyond the headline price and consider the total cost of ownership, which includes not only subscription fees but also implementation, training, and potential integration costs.
Subscription Models and Tiered Pricing
Most telehealth platforms operate on a subscription model, often with tiered pricing based on functionality or user volume. It’s critical to assess which tier best fits your practice’s current and projected needs.
- Per-Provider/Per-User: A fixed monthly fee per clinician or staff member accessing the platform.
- Per-Visit/Transaction: Charges incurred for each virtual consultation or completed transaction.
- Tiered Feature Sets: Different price points unlock varying levels of features, from basic video calls to advanced analytics and integrations.
- Enterprise Solutions: Custom pricing for larger organizations with specific needs and higher volumes.
Carefully read the fine print regarding overage charges, data storage limits, and additional fees for advanced features. A seemingly inexpensive base plan might become costly if your usage exceeds included allowances or if essential features are locked behind higher tiers.
Beyond the monthly fees, consider the long-term financial viability. A platform that offers scalability and flexible pricing can be more advantageous as your practice grows or its telehealth needs evolve. Transparency in pricing is a strong indicator of a trustworthy vendor.
Seamless Integration with Existing Systems
For US practices, the ability of a telehealth platform to integrate seamlessly with existing electronic health record (EHR) systems, billing software, and practice management tools is paramount. A truly effective telehealth platform comparison prioritizes integration to avoid data silos and inefficient workflows.
Poor integration can lead to duplicate data entry, increased administrative burden, and potential errors, ultimately hindering the benefits of telehealth. The goal is to create a unified ecosystem where patient information flows effortlessly between systems, improving accuracy and saving valuable staff time.
EHR and Practice Management Integration
The most critical integration is often with the EHR system. A robust integration ensures that patient demographics, medical history, and visit notes are easily accessible and updateable within the telehealth platform, and vice-versa.
- Bidirectional Data Flow: Allows data to be exchanged both ways, ensuring consistency across systems.
- Appointment Scheduling: Integrates with existing scheduling tools to streamline booking and reminders.
- Clinical Documentation: Enables direct charting within the telehealth platform or seamless transfer to the EHR.
- Prescription Management: Facilitates e-prescribing directly from the virtual visit interface.
Before committing to a platform, inquire about its specific integration capabilities with your current EHR and practice management software. Ask for case studies or references from practices using similar setups. The ease and depth of integration can be a significant differentiator between platforms.
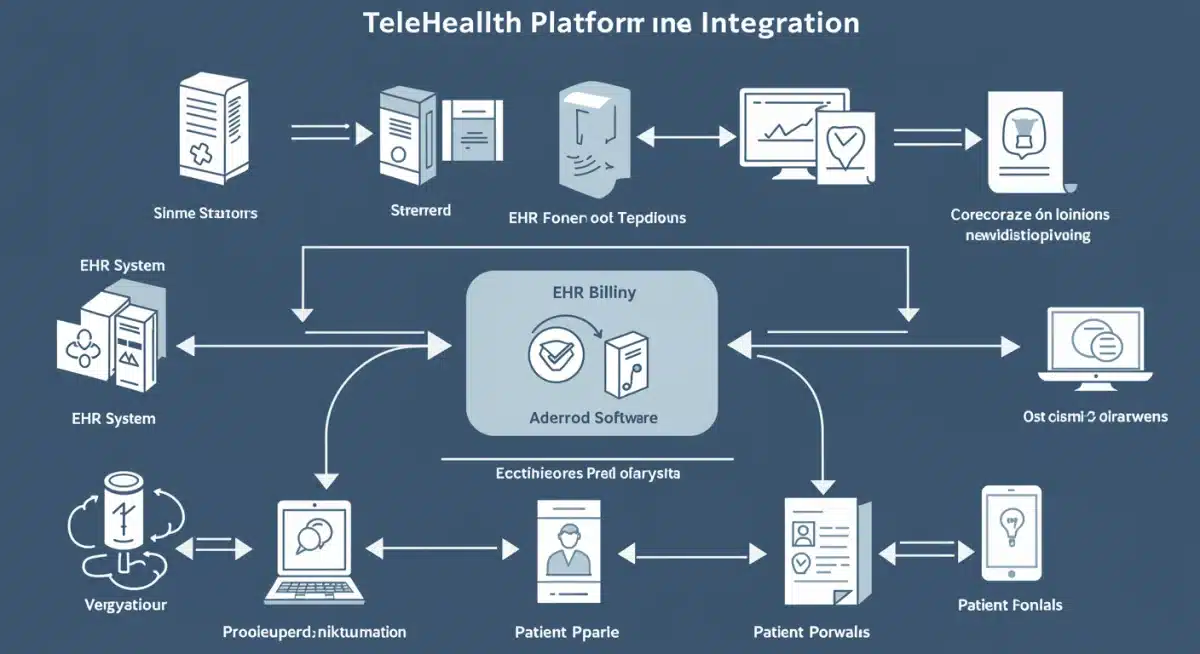
Beyond EHR, consider integration with billing systems to automate claims submission and payment processing. A well-integrated system minimizes manual tasks, reduces errors, and accelerates revenue cycles, directly impacting the practice’s financial health.
Assessing the Financial Impact and ROI
Evaluating the financial impact and return on investment (ROI) is a critical step in any telehealth platform comparison. For US practices, understanding how a telehealth solution can contribute to revenue generation, cost savings, and operational efficiencies is key to justifying the investment.
Telehealth offers multiple avenues for financial benefit, from reducing overhead costs to expanding patient reach. However, these benefits must be carefully quantified against the platform’s costs to determine a clear ROI. It’s not just about the upfront expenditure, but the long-term value created.
Revenue Generation and Cost Savings
Telehealth can significantly impact a practice’s bottom line by opening new revenue streams and reducing operational expenses.
- Expanded Patient Reach: Attracts patients from broader geographic areas or those with mobility issues.
- Reduced No-Show Rates: Virtual appointments often have lower no-show rates due to convenience.
- Optimized Provider Time: Allows clinicians to see more patients or manage their schedules more efficiently.
- Lower Overhead Costs: Potentially reduces the need for large physical office spaces and associated utilities.
- Improved Patient Retention: Offers flexibility that enhances patient satisfaction and loyalty.
Beyond direct financial gains, consider the indirect benefits. Enhanced patient access can lead to better health outcomes, reducing costly emergency room visits and hospitalizations. This, in turn, can positively impact a practice’s standing in value-based care models.
Calculating ROI involves a careful projection of increased revenue and decreased costs against the platform’s price. Practices should consider both tangible and intangible benefits, such as improved clinician morale and enhanced market competitiveness, when making their final decision.
Future-Proofing Your Telehealth Investment
As technology rapidly advances and healthcare needs evolve, selecting a telehealth platform in 2025 that is future-proof is essential. A telehealth platform comparison should not only focus on current functionalities but also on the vendor’s commitment to innovation, scalability, and adaptability. Investing in a platform that can grow with your practice ensures long-term viability and avoids costly migrations down the line.
The healthcare landscape is dynamic, with new regulations, technologies, and patient expectations constantly emerging. A platform that can seamlessly adapt to these changes will provide a sustainable advantage and protect your initial investment.
Scalability and Vendor Support
The ability of a platform to scale with your practice’s growth is a critical factor. Whether you anticipate adding more providers, expanding services, or increasing patient volume, the chosen solution should accommodate these changes without significant disruption or prohibitive costs.
- Scalable Infrastructure: Ensures the platform can handle increasing user loads and data volumes.
- Feature Roadmap: A clear vision from the vendor for future enhancements and new functionalities.
- Customer Support: Responsive and knowledgeable support is crucial for troubleshooting and maximizing platform utilization.
- API Accessibility: Allows for custom integrations with other tools as needed, providing greater flexibility.
Beyond technical scalability, evaluate the vendor’s reputation for reliability, security, and customer service. A strong partnership with your telehealth provider can be as important as the platform itself, offering peace of mind and continuous support.
Future-proofing also involves considering emerging technologies like AI-driven diagnostics, remote patient monitoring (RPM), and virtual reality (VR) for therapy. While not all practices may need these immediately, a platform that demonstrates a pathway to incorporate such innovations will be better positioned for the future.
| Key Aspect | Brief Description |
|---|---|
| Regulatory Compliance | Ensuring HIPAA, state-specific rules, and reimbursement policies are met is crucial for legal and financial stability. |
| Feature Set & UX | Evaluate core functionalities like video quality, secure messaging, and user-friendliness for both patients and providers. |
| Cost & ROI | Analyze pricing models, hidden fees, and potential for revenue growth and cost savings to determine overall financial benefit. |
| Integration Capabilities | Seamless connection with EHR, billing, and practice management systems is vital for efficient workflows and data integrity. |
Frequently Asked Questions About Telehealth Platforms
The most critical features include HIPAA-compliant video conferencing, secure messaging, seamless EHR integration, robust scheduling tools, and clear patient portals. These ensure both clinical effectiveness and operational efficiency for US practices.
Always verify that the platform vendor offers a Business Associate Agreement (BAA) and has strong security protocols, including encryption and access controls. Research their track record and any recent compliance audits or certifications for reassurance.
Costs typically involve monthly or annual subscription fees, often based on a per-provider or per-user model. Some platforms also include per-visit charges or tiered pricing that unlocks additional features. Always inquire about potential hidden fees.
EHR integration is vital for streamlined workflows, preventing duplicate data entry, and ensuring accurate patient records. It allows for seamless transfer of patient information, clinical notes, and billing data, significantly enhancing efficiency and reducing administrative burden.
Telehealth can boost revenue by expanding patient access, reducing no-show rates, and optimizing provider schedules. It also cuts costs associated with physical office space and administrative tasks, leading to a positive return on investment when strategically implemented.
Conclusion
The strategic selection of a telehealth platform in 2025 is a multifaceted decision for US practices, requiring a careful balance of features, cost, integration capabilities, and financial impact. By thoroughly evaluating these critical aspects, healthcare providers can choose a solution that not only meets their immediate needs but also positions them for long-term success in an increasingly digital healthcare environment. The right platform empowers practices to deliver high-quality, accessible care, enhance operational efficiency, and secure a robust financial future.