RPM Innovations: Q1 2026 Remote Patient Monitoring Updates

The future of remote patient monitoring in Q1 2026 is characterized by sophisticated device integration and AI-driven strategies that enhance patient engagement and deliver proactive healthcare solutions.
As we step into Q1 2026, the landscape of healthcare is being profoundly reshaped by advancements in remote patient monitoring 2026. This transformative shift is not merely about convenience; it represents a fundamental change in how chronic conditions are managed, acute care is delivered, and preventive health is prioritized across the United States.
The Evolution of Remote Patient Monitoring Devices
Remote patient monitoring (RPM) devices have undergone significant evolution, moving beyond basic vital sign trackers to sophisticated, multi-functional units. Q1 2026 sees the market flooded with innovative gadgets designed to offer more comprehensive and less intrusive monitoring for patients at home.
These new devices are not only more accurate but also integrate seamlessly into daily life, making compliance easier for patients. The focus has shifted from reactive data collection to proactive health management, often incorporating predictive analytics to flag potential issues before they become critical.
Wearable Technology and Smart Implants
Wearable RPM technology in 2026 extends far beyond smartwatches. We are seeing a rise in specialized patches, smart clothing, and even discreet, implantable sensors that provide continuous, high-fidelity data streams. These devices are designed for long-term use, offering insights into a patient’s health trends over time rather than just snapshots.
- Continuous Glucose Monitors (CGMs): Smaller, more accurate, and with extended wear times, CGMs are now seamlessly integrated with insulin pumps and AI-driven dosage recommendations.
- Smart Patches for Cardiac Monitoring: These adhesive patches offer multi-lead ECG monitoring, arrhythmia detection, and even early signs of heart failure, all without cumbersome wires.
- Bio-integrated Sensors: Miniaturized sensors capable of monitoring blood pressure, oxygen saturation, and even certain biomarkers directly from beneath the skin, wirelessly transmitting data.
The integration of these devices with personal health records and AI diagnostic tools is creating a truly interconnected healthcare ecosystem. This allows for personalized care plans that adapt in real-time to a patient’s physiological responses and lifestyle changes, marking a significant leap forward in preventative healthcare.
AI and Machine Learning: Driving Smarter RPM Strategies
Artificial intelligence (AI) and machine learning (ML) are no longer futuristic concepts in RPM; they are integral components of effective monitoring strategies in Q1 2026. These technologies are revolutionizing how patient data is interpreted, how risks are assessed, and how interventions are planned.
The sheer volume of data generated by modern RPM devices would be overwhelming without AI. Algorithms can sift through vast datasets, identify subtle patterns, and predict health deteriorations with remarkable accuracy, often surpassing human capabilities in early detection.
Predictive Analytics for Proactive Care
AI-powered predictive analytics are at the forefront of RPM strategies. By analyzing historical data, current vital signs, and patient-reported outcomes, AI models can forecast potential health crises, allowing clinicians to intervene proactively. This shifts the paradigm from treating illness to preventing it.
- Early Sepsis Detection: AI models can identify subtle physiological changes indicative of sepsis hours before traditional methods, enabling faster treatment and improved outcomes.
- Heart Failure Exacerbation Prediction: Machine learning algorithms analyze trends in weight, blood pressure, and activity levels to predict acute heart failure episodes, triggering timely adjustments to medication or lifestyle.
- Diabetic Complication Forecasting: AI integrates CGM data with dietary and activity logs to predict hyperglycemic or hypoglycemic events, providing personalized alerts and recommendations.
Furthermore, AI assists in optimizing resource allocation. By identifying patients who are at higher risk or require more frequent monitoring, healthcare providers can prioritize their attention and ensure that critical resources are directed where they are most needed, improving overall efficiency and patient satisfaction.
Enhanced Data Security and Privacy in RPM
With the increasing sophistication of remote patient monitoring 2026, the imperative for robust data security and patient privacy has never been greater. The healthcare industry is responding with advanced encryption, blockchain technology, and stringent regulatory compliance to protect sensitive health information.
Patients and providers alike must have absolute confidence that their data is secure from breaches and unauthorized access. This trust is foundational to the widespread adoption and success of RPM programs. Q1 2026 brings forward innovations specifically designed to fortify this trust.
Blockchain for Immutable Health Records
Blockchain technology is emerging as a powerful tool for creating immutable and transparent health records. Each piece of patient data, from vital signs to medication adherence, can be encrypted and stored on a distributed ledger, ensuring its integrity and preventing tampering.
- Enhanced Data Integrity: Blockchain ensures that once data is recorded, it cannot be altered, providing a reliable audit trail for all health information.
- Secure Data Sharing: Patients can grant granular access to their health data to specific providers or researchers, with every access logged and verifiable.
- Decentralized Record Keeping: Reduces reliance on single points of failure, making the system more resilient to cyberattacks and data loss.
Beyond blockchain, advanced biometric authentication, end-to-end encryption for data transmission, and regular security audits are standard practices. Regulatory bodies are also adapting swiftly, with updated guidelines and compliance frameworks to keep pace with technological advancements and safeguard patient information effectively.
Interoperability and Seamless Integration with EHRs
A significant challenge in RPM has always been the fragmentation of data across various devices and electronic health records (EHRs). In Q1 2026, a strong emphasis is placed on achieving true interoperability, ensuring that RPM data flows seamlessly into a patient’s comprehensive health profile.
This integration is crucial for providing a holistic view of patient health, enabling clinicians to make informed decisions without having to manually collate information from disparate sources. The goal is to create a unified data ecosystem that supports efficient and coordinated care.
Standardized Data Exchange Protocols
The adoption of standardized data exchange protocols, such as FHIR (Fast Healthcare Interoperability Resources), is accelerating. These protocols facilitate the secure and efficient exchange of health information between different systems, regardless of their underlying technology.
- Unified Patient View: All RPM data, lab results, medication history, and clinical notes are consolidated into a single, accessible EHR, providing a complete patient narrative.
- Reduced Administrative Burden: Automated data transfer eliminates manual entry, freeing up healthcare professionals to focus on patient care rather than data management.
- Improved Clinical Decision Support: With all relevant data at their fingertips, clinicians can leverage AI-powered decision support tools more effectively, leading to better diagnostic accuracy and treatment planning.
Furthermore, cloud-based platforms are playing a pivotal role in achieving this interoperability. By hosting RPM data and EHRs in secure cloud environments, healthcare organizations can ensure accessibility, scalability, and real-time synchronization across their entire network, benefiting both providers and patients.
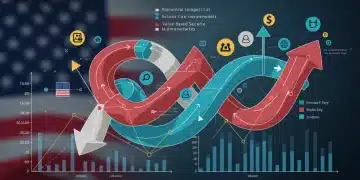
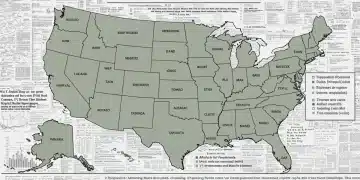
Reimbursement Models and Policy Shifts in the US
The financial viability and widespread adoption of remote patient monitoring 2026 are heavily influenced by evolving reimbursement models and healthcare policy in the United States. Q1 2026 has seen crucial updates aimed at incentivizing RPM adoption and ensuring fair compensation for providers.
Understanding these policy shifts is critical for healthcare organizations looking to implement or expand their RPM programs. The aim is to create a sustainable framework that supports innovation while ensuring equitable access to care for all Americans, especially those in underserved areas.
CMS Updates and Commercial Payer Policies
The Centers for Medicare & Medicaid Services (CMS) continues to refine its RPM reimbursement codes, expanding coverage and clarifying billing guidelines. Commercial payers are also increasingly recognizing the value of RPM, integrating it into their benefit plans.
- Expanded CPT Codes: New CPT codes are being introduced or existing ones updated to cover a broader range of RPM services, including AI-driven analytics and specialized device monitoring.
- Value-Based Care Alignment: Reimbursement models are increasingly linked to value-based care outcomes, rewarding providers for improved patient health and reduced hospital readmissions through RPM.
- State-Level Initiatives: Several states are implementing their own RPM incentive programs, often targeting specific chronic conditions or rural populations to address health disparities.
These policy changes reflect a growing consensus on the efficacy and cost-effectiveness of RPM. As evidence mounts regarding its ability to improve patient outcomes and reduce healthcare expenditures, we can anticipate continued favorable policy adjustments that will further cement RPM’s role in mainstream healthcare delivery.
Patient Engagement and User Experience in RPM
The success of remote patient monitoring 2026 hinges not just on technological prowess, but crucially on patient engagement and a seamless user experience. Devices and platforms must be intuitive, accessible, and motivating to ensure consistent adherence and optimal health outcomes.
In Q1 2026, the focus is squarely on designing RPM solutions that empower patients, making them active participants in their own health management. This includes user-friendly interfaces, personalized feedback, and strong communication channels with their care teams.
Gamification and Personalized Feedback
To boost engagement, many RPM platforms are incorporating gamification elements, rewarding patients for adherence to monitoring schedules and health goals. Personalized feedback, delivered through easy-to-understand dashboards and alerts, helps patients grasp their health status and progress.
- Intuitive Mobile Apps: Companion mobile applications are designed with simple navigation, clear data visualization, and immediate access to support resources.
- Virtual Health Coaches: AI-powered virtual coaches provide encouragement, answer common questions, and offer tailored health tips based on individual monitoring data.
- Family Caregiver Portals: Secure portals allow authorized family members to view patient data and communicate with the care team, fostering a supportive environment.
Ultimately, the goal is to make RPM an integral yet unobtrusive part of a patient’s life. By focusing on design that prioritizes ease of use, clear communication, and motivational tools, healthcare providers can cultivate higher patient satisfaction and achieve sustained engagement, leading to better long-term health management.
| Key Aspect | Description in Q1 2026 |
|---|---|
| Device Innovation | Advanced wearables, smart implants, and multi-functional sensors offering comprehensive, less intrusive monitoring. |
| AI Integration | AI and ML for predictive analytics, early detection of health deteriorations, and optimized resource allocation. |
| Data Security | Robust measures including blockchain, end-to-end encryption, and updated regulatory frameworks protecting patient data. |
| Policy & Reimbursement | Evolving CMS and commercial payer policies incentivize RPM, aligning with value-based care and state initiatives. |
Frequently Asked Questions About Remote Patient Monitoring in Q1 2026
Q1 2026 has introduced advanced wearable patches for multi-lead ECG and continuous glucose monitoring, along with discreet bio-integrated sensors. These devices offer enhanced accuracy and seamless integration, moving towards proactive health management rather than reactive data collection.
AI and machine learning are crucial for predictive analytics, identifying subtle patterns in patient data to forecast potential health crises. This enables clinicians to intervene proactively, improving early detection for conditions like sepsis and heart failure exacerbations, and optimizing resource allocation.
Data security in RPM for Q1 2026 is bolstered by advanced encryption, blockchain technology for immutable health records, and stringent regulatory compliance. These measures ensure data integrity, secure sharing, and protection against cyber threats, fostering patient and provider trust.
Yes, a key focus in Q1 2026 is achieving true interoperability. Standardized data exchange protocols like FHIR are enabling seamless integration of RPM data into electronic health records (EHRs). This provides a unified patient view, reduces administrative burden, and enhances clinical decision support.
CMS and commercial payers are updating reimbursement codes and policies to incentivize RPM adoption in 2026. These changes align with value-based care, expanding coverage for a broader range of services and encouraging state-level initiatives to improve patient outcomes and reduce healthcare costs.
Conclusion
The first quarter of 2026 marks a pivotal moment in the evolution of remote patient monitoring. With sophisticated new devices, advanced AI-driven strategies, robust data security protocols, and increasingly favorable reimbursement policies, RPM is firmly establishing itself as an indispensable component of modern healthcare. The emphasis on patient engagement and seamless integration ensures that these technological advancements translate into tangible improvements in health outcomes and a more efficient, patient-centered healthcare system across the United States. As MedTech continues to grow, the future of healthcare looks increasingly connected and proactive.