CMS Telehealth Reimbursement 2025: Expert Analysis

The Centers for Medicare & Medicaid Services (CMS) are set to introduce significant adjustments to telehealth reimbursement in 2025, profoundly shaping access to virtual healthcare and impacting providers across the United States.
As the healthcare landscape continues its rapid evolution, particularly with the sustained growth of virtual care, keeping pace with regulatory shifts is paramount. For healthcare providers, administrators, and patients alike, Understanding the Latest CMS Reimbursement Adjustments for Telehealth in 2025: An Expert Analysis is not just important, it’s critical for navigating the future of accessible healthcare in the United States.
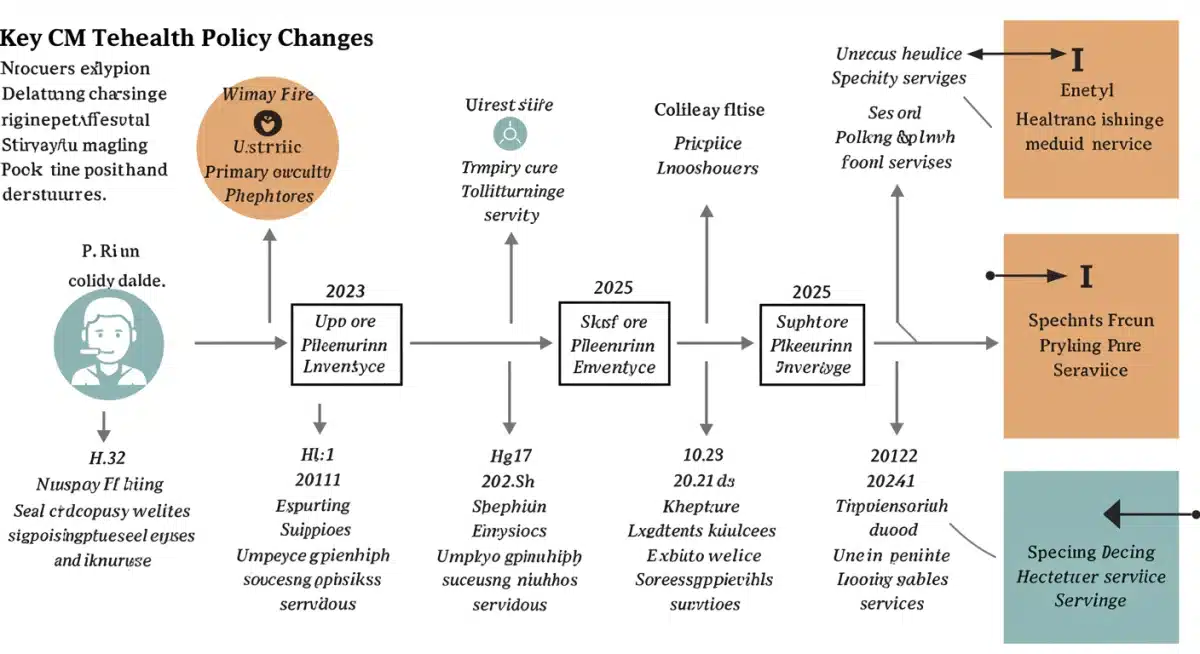
The evolving landscape of telehealth reimbursement
Telehealth has rapidly transformed from a niche service to an integral component of healthcare delivery, accelerated by the COVID-19 pandemic. The Centers for Medicare & Medicaid Services (CMS) played a pivotal role in this expansion by temporarily waiving numerous restrictions and broadening reimbursement for virtual services. However, as the public health emergency recedes, CMS is meticulously re-evaluating these temporary measures, leading to significant adjustments for 2025.
These forthcoming changes are designed to balance continued access to care with program integrity and fiscal responsibility. Stakeholders across the healthcare spectrum, from large hospital systems to independent practitioners and technology innovators, must understand these shifts to adapt their strategies effectively. The goal is to establish a sustainable framework that supports high-quality, cost-effective virtual care for Medicare beneficiaries.
Key drivers behind the 2025 adjustments
- Post-PHE evaluation: CMS is analyzing data from the public health emergency to determine which flexibilities should be made permanent.
- Program integrity concerns: Efforts to prevent fraud, waste, and abuse in telehealth services are driving stricter regulations.
- Provider feedback: Input from healthcare professionals regarding the practical application and efficacy of telehealth is being considered.
- Patient access and equity: Ensuring that telehealth remains accessible to diverse populations, including those in rural and underserved areas, is a core objective.
The adjustments reflect a maturing understanding of telehealth’s capabilities and limitations, moving beyond emergency responses to a more structured, long-term policy. This evolution requires careful consideration of how virtual care integrates with traditional in-person services, ensuring a seamless and effective patient experience.
In conclusion, the 2025 CMS telehealth reimbursement adjustments are a natural progression in the integration of virtual care into the broader healthcare system. They signal a move towards a more permanent and regulated telehealth environment, necessitating proactive adaptation from all involved parties to maintain service quality and financial viability.
Understanding the proposed changes for 2025
The proposed CMS reimbursement adjustments for telehealth in 2025 encompass several critical areas, impacting how providers are compensated for virtual services. These changes aim to refine existing policies, introduce new payment models, and clarify service eligibility, all while maintaining a focus on patient outcomes and cost-efficiency.
One of the most anticipated changes involves the permanent extension of certain telehealth services that were temporarily covered during the public health emergency. However, this extension often comes with revised payment rates or new conditions. Providers need to meticulously review the specific Current Procedural Terminology (CPT) codes affected and understand any new documentation requirements to ensure compliance and avoid reimbursement denials.
Specific service coverage modifications
- Audio-only services: While some audio-only services may retain coverage, CMS is expected to tighten restrictions, emphasizing the need for synchronous audio-visual communication where clinically appropriate.
- Mental health services: Telehealth for mental health is likely to see continued strong support, potentially with specific provisions to ensure continuity of care.
- Originating site requirements: Although many originating site restrictions were waived, CMS may reintroduce some limitations or establish new definitions for eligible originating sites, particularly for certain types of services.
Furthermore, CMS is exploring new payment methodologies, including value-based care models that integrate telehealth. These models could link reimbursement to quality metrics and patient outcomes rather than solely fee-for-service, encouraging a more holistic approach to virtual care delivery. Such shifts require providers to invest in robust data collection and reporting capabilities.
The proposed changes also address concerns about the appropriate use of telehealth, particularly regarding the distinction between medically necessary services and those that could be effectively delivered in-person. This scrutiny is part of a broader effort to optimize resource allocation and ensure that telehealth truly enhances, rather than merely substitutes, traditional care.
Ultimately, the 2025 adjustments are poised to solidify telehealth’s place in the U.S. healthcare system. Providers must engage with the proposed rules, offering feedback during public comment periods, and begin preparing their operational and billing processes for the upcoming changes to ensure a smooth transition and continued financial stability.
Impact on providers: financial and operational considerations
The CMS reimbursement adjustments for telehealth in 2025 will undoubtedly have profound financial and operational implications for healthcare providers. Understanding these impacts is crucial for strategic planning and ensuring the sustainability of virtual care offerings. Providers must assess how changes to payment rates, service coverage, and documentation requirements will affect their revenue streams and cost structures.
Financially, a primary concern for many providers is the potential for reduced reimbursement rates for certain telehealth services. While the expansion of telehealth brought significant revenue opportunities, the normalization of these services may lead to more conservative payment models. This could necessitate a re-evaluation of staffing models, technology investments, and overall service delivery strategies to maintain profitability.
Operational adjustments for telehealth integration
- Technology infrastructure: Providers may need to upgrade their telehealth platforms to meet new security, interoperability, and documentation standards.
- Staff training: Clinical and administrative staff will require ongoing training on updated billing codes, compliance guidelines, and best practices for virtual encounters.
- Workflow optimization: Re-engineering patient intake, scheduling, and follow-up processes to seamlessly integrate telehealth into existing workflows will be essential.
Operationally, the adjustments could require significant changes to how telehealth services are delivered and managed. Stricter documentation requirements, for instance, will demand more detailed record-keeping to justify the medical necessity and appropriateness of virtual visits. This might involve new templates in Electronic Health Records (EHR) systems and enhanced training for clinicians on proper charting for telehealth.
Furthermore, providers might need to revisit their patient engagement strategies to ensure that patients understand when telehealth is an appropriate option and what to expect from virtual appointments. Clear communication about service availability, technology requirements, and billing practices will be vital for patient satisfaction and adherence.
In essence, the 2025 adjustments call for a proactive and adaptive approach from providers. Those who anticipate and strategically prepare for these changes by investing in technology, staff training, and robust compliance programs will be better positioned to thrive in the evolving telehealth landscape while continuing to deliver high-quality patient care.
The patient perspective: access, equity, and quality of care
While CMS reimbursement adjustments primarily target providers, their ultimate impact reverberates directly through the patient experience. For Medicare beneficiaries, the 2025 changes will influence access to care, the equity of telehealth services, and the perceived quality of virtual encounters. Ensuring that these adjustments do not inadvertently create barriers to care, especially for vulnerable populations, is a critical consideration.
Access to telehealth has been a game-changer for many, particularly those in rural areas, individuals with mobility challenges, or patients seeking specialized care not readily available locally. The permanence of certain telehealth services is a positive step, but any reintroduction of originating site restrictions or significant reductions in audio-only coverage could disproportionately affect patients with limited internet access or technological literacy.
Ensuring equitable access to virtual care
- Digital literacy programs: Initiatives to educate patients on how to use telehealth platforms effectively are crucial.
- Broadband infrastructure: Continued advocacy for expanding high-speed internet access in underserved areas remains vital.
- Language and cultural considerations: Telehealth services must be culturally competent and available in multiple languages to serve diverse patient populations.
The quality of care delivered via telehealth is another paramount concern. Patients expect the same level of diagnostic accuracy, empathetic communication, and comprehensive treatment planning in a virtual setting as they would receive in person. CMS’s focus on appropriate utilization and documentation aims to reinforce the medical necessity and clinical efficacy of telehealth services, thereby safeguarding patient trust and outcomes.
Moreover, patient education about the types of services available through telehealth and what constitutes an appropriate virtual visit will be essential. Clear guidelines can help manage patient expectations and ensure they utilize telehealth effectively, reserving in-person visits for conditions that truly require physical examination or advanced procedures.
Ultimately, the success of the 2025 CMS adjustments, from a patient perspective, will hinge on their ability to maintain broad access to necessary care, promote health equity, and uphold high standards of quality, all while adapting to the evolving technological capabilities and clinical best practices in virtual health.
Technological advancements and telehealth integration
The ongoing evolution of telehealth is inextricably linked to advancements in technology. As CMS refines its reimbursement policies for 2025, the role of robust and innovative technological solutions becomes even more critical. Providers must leverage these advancements not only to meet new compliance standards but also to enhance the efficiency, security, and effectiveness of their virtual care offerings.
Interoperability, for instance, is a key focus. Seamless integration between telehealth platforms, Electronic Health Records (EHRs), and other health information systems is essential for accurate documentation, billing, and continuity of care. The ability to easily share patient data across different systems minimizes administrative burden and reduces the risk of errors, which will be increasingly important under stricter reimbursement rules.
Innovations driving the future of telehealth
- Remote patient monitoring (RPM): Advanced RPM devices and platforms allow for continuous tracking of vital signs and other health metrics, enabling proactive interventions and potentially expanding reimbursable services.
- Artificial intelligence (AI) and machine learning (ML): AI can assist with diagnostic support, personalized treatment plans, and identifying patients who would benefit most from telehealth interventions, streamlining provider workflows.
- Enhanced cybersecurity: With increased data exchange, sophisticated cybersecurity measures are paramount to protect patient privacy and comply with HIPAA regulations, a non-negotiable aspect of telehealth.
Furthermore, the user experience for both providers and patients is being continuously improved through more intuitive interfaces, better video and audio quality, and integrated communication tools. These enhancements contribute to more effective virtual consultations and higher patient satisfaction, which can indirectly impact reimbursement through better patient engagement and adherence.
The 2025 adjustments also highlight the need for scalable and secure telehealth infrastructure. As virtual care becomes a permanent fixture, providers must invest in solutions that can handle increasing patient volumes while maintaining data integrity and system reliability. This includes cloud-based solutions that offer flexibility and robust disaster recovery capabilities.
In summary, technological innovation is not just supportive of telehealth; it is foundational to its continued growth and compliance with evolving CMS regulations. Providers who embrace and strategically implement cutting-edge technologies will be better positioned to navigate the 2025 reimbursement landscape and deliver superior virtual care.
Preparing for the 2025 CMS reimbursement changes
Proactive preparation is paramount for healthcare organizations to successfully navigate the CMS telehealth reimbursement adjustments slated for 2025. Waiting until the last minute can lead to significant financial disruptions, compliance issues, and a reduction in the quality of patient care. A multi-faceted approach involving policy review, operational adjustments, and technological readiness is essential.
The first step involves a comprehensive review of all proposed and final CMS rules pertaining to telehealth for 2025. This includes understanding changes to CPT codes, eligible services, originating and distant site requirements, and documentation standards. Providers should identify which of their current telehealth offerings will be most affected and begin planning for necessary modifications.
Strategic steps for readiness
- Financial modeling: Analyze the potential financial impact of new reimbursement rates and adjust budgeting and revenue projections accordingly.
- Compliance audits: Conduct internal audits of current telehealth billing and documentation practices to identify and rectify any areas of non-compliance before the new rules take effect.
- Stakeholder engagement: Communicate proactively with staff, patients, and technology vendors about upcoming changes to ensure everyone is informed and prepared.
Operational preparedness extends to staff training. Clinical and administrative teams must be thoroughly educated on the updated billing codes, new documentation requirements, and any changes in patient eligibility or service delivery protocols. Refresher courses and clear internal guidelines can help ensure consistency and accuracy across the organization.
Furthermore, engaging with professional organizations and industry groups can provide valuable insights and advocacy opportunities. These groups often offer webinars, whitepapers, and forums to discuss the implications of new policies and share best practices for adaptation. Collaboration can help providers stay ahead of the curve and collectively influence future policy directions.
In conclusion, successful preparation for the 2025 CMS telehealth reimbursement changes is an ongoing process that requires diligent attention to detail, strategic foresight, and a commitment to continuous improvement. By taking these proactive steps, healthcare providers can ensure they remain compliant, financially stable, and capable of delivering high-quality virtual care to their patients.
Future outlook: sustainability and innovation in telehealth
As the healthcare industry moves beyond the immediate post-pandemic phase, the future of telehealth under the 2025 CMS reimbursement adjustments points towards a landscape focused on sustainability and continuous innovation. The goal is no longer just to expand access, but to integrate virtual care more deeply into the healthcare ecosystem, ensuring its long-term viability and effectiveness.
Sustainable telehealth models will emphasize appropriate utilization, ensuring that virtual services are delivered when clinically beneficial and cost-effective. This means a sharper focus on outcomes, patient satisfaction, and the prevention of unnecessary services. CMS’s adjustments are a step towards refining this balance, encouraging providers to think strategically about how telehealth complements traditional care.
Trends shaping telehealth’s future
- Hybrid care models: A blend of in-person and virtual visits will become the norm, requiring seamless coordination and integrated systems.
- Specialized telehealth: Growth in niche areas such as tele-dermatology, tele-ophthalmology, and remote physical therapy, driven by technological enhancements and provider expertise.
- Global health integration: Lessons learned from domestic telehealth expansion could influence international healthcare policies and cross-border care delivery.
Innovation will continue to be a driving force, particularly in areas like artificial intelligence, wearable devices, and advanced data analytics. These technologies will enable more personalized care, predictive analytics for disease management, and more efficient administrative processes. The reimbursement framework needs to evolve to support and incentivize the adoption of such innovations, rather than hinder them.
Policy advocacy will also play a crucial role. Healthcare stakeholders must continue to engage with policymakers to ensure that future regulations foster innovation and address the evolving needs of both providers and patients. This collaborative approach can help shape a regulatory environment that is responsive and forward-thinking.
Ultimately, the 2025 CMS reimbursement adjustments are not an endpoint but a significant milestone in the journey of telehealth. The future promises a more integrated, technologically advanced, and patient-centric virtual care system, provided that continuous adaptation, thoughtful policy, and unwavering commitment to quality remain at the forefront.
| Key Aspect | Brief Description |
|---|---|
| Policy Evolution | CMS is moving from temporary pandemic waivers to a more permanent, structured telehealth reimbursement framework for 2025. |
| Provider Impact | Changes affect payment rates, service coverage, and documentation, requiring financial and operational adjustments for healthcare providers. |
| Patient Considerations | Adjustments will influence access, equity, and quality of virtual care for Medicare beneficiaries, emphasizing digital literacy and broadband. |
| Technological Role | Advanced tech like RPM, AI, and robust cybersecurity are crucial for meeting new compliance standards and enhancing telehealth effectiveness. |
Frequently asked questions about CMS telehealth 2025 changes
CMS aims to balance continued patient access to virtual care with program integrity and fiscal responsibility. The adjustments seek to establish a sustainable, long-term framework for telehealth, moving beyond temporary pandemic measures to integrate virtual services more permanently into the healthcare system while maintaining quality.
While some audio-only services might retain coverage, CMS is expected to introduce stricter guidelines. The emphasis will likely shift towards synchronous audio-visual communication where clinically appropriate, potentially limiting the scope and reimbursement for services delivered solely via audio.
Providers should prepare for updated documentation requirements, potential adjustments to payment rates, and the need for enhanced technology infrastructure. Staff training on new billing codes and compliance guidelines, along with workflow optimization, will be crucial for a smooth transition and continued financial stability.
Maintaining access for rural and underserved populations is a core objective for CMS. While some originating site rules may be refined, efforts are expected to ensure telehealth remains a viable option. Continued advocacy for broadband expansion and digital literacy programs will support equitable access.
Technology plays a vital role through improved interoperability with EHRs, advanced remote patient monitoring, and enhanced cybersecurity measures. AI and machine learning can also streamline administrative tasks and improve diagnostic support, helping providers meet new compliance and efficiency standards effectively.
Conclusion
The Centers for Medicare & Medicaid Services’ reimbursement adjustments for telehealth in 2025 represent a pivotal moment in the evolution of virtual care within the United States. These changes, born from careful evaluation of pandemic-era flexibilities and a commitment to long-term sustainability, will reshape financial models for providers, influence patient access and equity, and accelerate the adoption of innovative technological solutions. Proactive engagement, strategic planning, and a deep understanding of the revised policies will be essential for all stakeholders to navigate this evolving landscape successfully, ensuring that telehealth continues to deliver high-quality, accessible care for Medicare beneficiaries.