MedTech Clinical Validation: 12-Month Insider Strategies

MedTech startups can achieve clinical validation within 12 months by employing strategic regulatory engagement, early clinical trial design, robust data management, and agile development, accelerating market entry and patient impact.
Navigating the complex landscape of MedTech development can be daunting, especially when aiming for rapid market entry. This article delves into the MedTech Clinical Validation process, offering insider strategies to achieve this crucial milestone within a challenging 12-month timeframe.
Understanding the 12-Month Validation Imperative
For MedTech startups, time is often the most critical resource. The pressure to validate a device or solution quickly stems from various factors, including investor expectations, market competition, and the urgent need to address unmet clinical needs. Achieving clinical validation within 12 months is an ambitious goal, but entirely achievable with a meticulously planned and executed strategy.
This aggressive timeline demands an integrated approach, where every phase, from preclinical studies to regulatory submissions, is streamlined and optimized for efficiency. It requires a deep understanding of regulatory pathways, proactive stakeholder engagement, and a commitment to data-driven decision-making. The ability to pivot and adapt based on early feedback is also paramount to staying on schedule.
Strategic Planning and Early Engagement
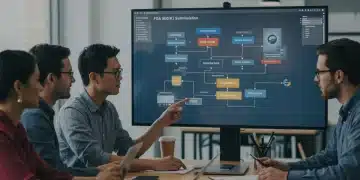
The foundation of rapid clinical validation lies in comprehensive strategic planning. This isn’t just about outlining tasks, but about foreseeing potential roadblocks and building contingencies. Early engagement with regulatory bodies and key opinion leaders can significantly shorten timelines.
- Regulatory Pathway Mapping: Identify the most appropriate regulatory pathway (e.g., 510(k), De Novo, PMA) early on.
- Pre-Submission Meetings: Engage with the FDA or other relevant bodies through pre-submission meetings to clarify requirements and address potential concerns.
- Key Opinion Leader (KOL) Input: Involve KOLs from the outset to refine study design and ensure clinical relevance.
By front-loading these critical activities, startups can mitigate risks and gain valuable insights that inform subsequent development stages, ultimately accelerating the validation process. A clear roadmap, coupled with expert guidance, helps avoid costly delays and ensures alignment with regulatory expectations.
Designing Agile Clinical Trials for Speed
Traditional clinical trial designs can be lengthy and resource-intensive, often exceeding a 12-month window. To meet an aggressive timeline, MedTech startups must embrace agile methodologies, focusing on lean study designs that yield statistically significant data efficiently. This involves careful patient selection, optimized endpoints, and continuous data monitoring.
An agile approach prioritizes rapid iteration and learning, allowing for adjustments to the trial protocol as data emerges. This doesn’t mean compromising scientific rigor; rather, it emphasizes smart design choices that maximize data collection effectiveness while minimizing unnecessary complexity. The goal is to gather sufficient evidence for safety and efficacy without over-burdening the process.
Leveraging Real-World Evidence (RWE)
The integration of real-world evidence (RWE) is increasingly recognized as a powerful tool to complement traditional clinical trial data. RWE, derived from electronic health records, claims data, and patient registries, can provide valuable insights into device performance in diverse patient populations and real-world settings, potentially accelerating validation.
- Pilot Studies: Conduct small, focused pilot studies to gather preliminary safety and performance data quickly.
- Adaptive Trial Designs: Utilize adaptive trial designs where sample sizes or treatment arms can be modified based on interim analysis, optimizing resource allocation.
- Digital Health Integration: Employ digital health tools for remote monitoring and data collection, enhancing efficiency and patient engagement.
By strategically incorporating RWE and adopting adaptive trial designs, startups can generate robust evidence more rapidly, demonstrating the value of their innovation to both regulators and clinicians. This innovative approach allows for a more dynamic and responsive validation process.
Mastering Regulatory Navigation and Documentation
Effective regulatory navigation is not merely about compliance; it’s about strategic engagement and meticulous documentation. Understanding the nuances of FDA requirements, preparing a compelling submission, and maintaining open communication with regulators are paramount for timely approval. Any misstep in this phase can lead to significant delays.
The documentation process itself should be viewed as an ongoing effort, not a last-minute scramble. Building a comprehensive regulatory dossier systematically ensures that all necessary information is readily available and presented clearly. This proactive approach minimizes the chances of information requests from regulatory bodies, which can extend review cycles.
Pre-market Submission Excellence
A well-prepared pre-market submission is a cornerstone of rapid validation. This involves not only presenting robust clinical data but also demonstrating a thorough understanding of the device’s design, manufacturing, and quality control processes. Clarity, conciseness, and accuracy are critical in all submission documents.
- Q-Submission Meetings: Utilize Q-submission meetings to get early feedback on specific aspects of your submission package.
- Robust Quality Management System (QMS): Implement a strong QMS from day one to ensure compliance and traceability of all development activities.
- Expert Regulatory Affairs Team: Assemble or consult with a highly experienced regulatory affairs team to guide the submission process.
By investing in a high-quality submission and maintaining a proactive dialogue with regulatory agencies, MedTech startups can significantly de-risk the validation process and accelerate their time to market. This meticulous attention to detail can be the difference between timely approval and prolonged review.
Data Management and Biostatistics for Accelerated Insights
In the pursuit of rapid clinical validation, efficient data management and robust biostatistical analysis are non-negotiable. The ability to collect, process, and interpret data quickly and accurately directly impacts the speed of insights and decision-making. Poor data practices can lead to unreliable results and regulatory scrutiny, jeopardizing the entire timeline.
Implementing a comprehensive data management plan from the outset, including secure data capture systems and clear data governance policies, is essential. Furthermore, engaging biostatisticians early in the trial design phase ensures that the study is powered correctly and that the data collected will be amenable to rigorous analysis, supporting a swift validation.

Real-Time Data Monitoring and Analysis
Moving beyond traditional batch processing, real-time data monitoring and analysis can dramatically accelerate the identification of trends, potential issues, and key findings. This allows for immediate adjustments to the trial protocol or even early termination if efficacy or safety thresholds are met, saving time and resources.
- Electronic Data Capture (EDC) Systems: Utilize advanced EDC systems for efficient and secure data collection.
- Interim Analysis: Plan for scheduled interim analyses to evaluate progress and make informed decisions on trial continuation or modification.
- Statistical Expertise: Ensure access to experienced biostatisticians who can perform rapid and accurate data interpretation.
By embracing real-time data strategies and leveraging expert statistical support, MedTech startups can transform raw data into actionable insights with unprecedented speed, thereby fueling a faster clinical validation process. This proactive approach ensures data integrity and accelerates the path to regulatory approval.
Building a Cross-Functional Validation Team
Achieving clinical validation within 12 months is a team sport. It requires seamless collaboration among diverse experts, including clinicians, engineers, regulatory affairs specialists, biostatisticians, and project managers. A siloed approach will inevitably lead to communication breakdowns and delays. A dedicated, cross-functional team, empowered to make rapid decisions, is crucial.
Effective team communication and a shared understanding of the overarching goals are fundamental. Regular meetings, clear lines of responsibility, and a culture of accountability ensure that everyone is aligned and working towards the same aggressive timeline. The ability to quickly resolve conflicts and adapt to unforeseen challenges is a hallmark of a high-performing validation team.
Fostering a Culture of Agility and Collaboration
Beyond individual expertise, the organizational culture must support the rapid pace required for 12-month validation. This means fostering an environment where agility, open communication, and problem-solving are celebrated. Leaders must empower their teams, trust their judgment, and provide the resources necessary to overcome hurdles swiftly.
- Dedicated Project Manager: Appoint a skilled project manager to oversee all aspects of the validation process, ensuring milestones are met.
- Interdisciplinary Training: Provide cross-training to team members to foster a broader understanding of different functional areas.
- Regular Communication Cadence: Establish a consistent schedule for team meetings and updates to maintain alignment and address issues promptly.
A well-integrated, collaborative, and agile team is the engine that drives rapid clinical validation. By investing in team building and fostering a supportive culture, MedTech startups can significantly enhance their chances of meeting ambitious timelines. This collective effort is key to navigating the complexities of regulatory approval.
Post-Market Surveillance and Continuous Improvement
While the focus is often on pre-market clinical validation, a savvy MedTech startup understands that the journey doesn’t end with regulatory approval. Post-market surveillance (PMS) is not only a regulatory requirement but also a critical component of continuous product improvement and long-term success. It provides valuable real-world performance data that can inform future iterations and expand indications.
Integrating PMS planning into the initial development phases ensures that the necessary systems and processes are in place from day one. This includes establishing robust complaint handling mechanisms, developing post-market study protocols, and maintaining an active dialogue with users and patients. This holistic view of the product lifecycle reinforces trust and demonstrates a commitment to patient safety.
Leveraging Feedback for Iterative Development
The data gathered through post-market surveillance is a goldmine for iterative development. By systematically collecting and analyzing real-world feedback, startups can identify areas for improvement, address unforeseen challenges, and enhance the overall user experience. This continuous feedback loop is vital for maintaining a competitive edge and ensuring long-term market relevance.
- User Feedback Mechanisms: Implement clear channels for collecting user and patient feedback, such as surveys, focus groups, and direct support.
- Adverse Event Reporting: Establish a robust system for tracking and reporting adverse events in compliance with regulatory requirements.
- Post-Market Clinical Follow-up (PMCF): Conduct PMCF studies to gather additional clinical data on long-term performance and safety.
By embracing post-market surveillance as an integral part of their strategy, MedTech startups not only fulfill regulatory obligations but also create a pathway for continuous innovation and product refinement. This commitment to ongoing improvement strengthens their market position and ultimately benefits patient care. PMS closes the loop on the validation journey, ensuring sustained excellence.
| Key Strategy | Brief Description |
|---|---|
| Early Regulatory Engagement | Proactively engage with regulatory bodies (e.g., FDA) through pre-submission meetings to clarify requirements and optimize pathways. |
| Agile Trial Design | Employ lean, adaptive clinical trial methodologies and integrate real-world evidence to accelerate data collection and analysis. |
| Robust Data Management | Implement real-time data monitoring and expert biostatistical analysis for rapid, accurate insights and decision-making. |
| Cross-Functional Teams | Foster collaboration among diverse experts and empower teams for swift problem-solving and decision-making. |
Frequently Asked Questions About MedTech Clinical Validation
The primary challenge is balancing regulatory rigor with aggressive timelines. Startups must navigate complex FDA requirements while rapidly generating robust safety and efficacy data, often with limited resources. Strategic planning and early regulatory engagement are crucial to overcome this.
Early engagement, such as pre-submission meetings, allows startups to clarify regulatory expectations, address potential concerns, and gain valuable feedback on their development plan. This proactive approach minimizes unforeseen issues and can significantly reduce review cycles.
Real-world evidence (RWE) complements traditional clinical trial data by providing insights into device performance in diverse, real-world settings. When strategically integrated, RWE can strengthen a submission, validate initial findings, and potentially accelerate regulatory decisions.
A cross-functional team ensures all critical aspects—clinical, engineering, regulatory, statistical—are integrated and aligned. This prevents silos, fosters efficient problem-solving, and facilitates rapid decision-making, which is vital for meeting tight validation deadlines.
After initial clinical validation, post-market surveillance becomes crucial. This involves continuous monitoring for safety and performance, collecting user feedback, and fulfilling ongoing regulatory requirements. It also informs iterative product improvements and potential new indications.
Conclusion
Achieving clinical validation for MedTech products within an ambitious 12-month window is a testament to strategic foresight, meticulous execution, and unwavering dedication. By prioritizing early regulatory engagement, embracing agile clinical trial designs, leveraging robust data management, and fostering a collaborative, cross-functional team environment, startups can navigate the complexities of the healthcare landscape with greater efficiency. The journey doesn’t end with approval; a commitment to post-market surveillance ensures continuous improvement and long-term success, ultimately bringing transformative innovations to patients faster. These insider strategies provide a comprehensive roadmap for MedTech startups aiming to make a significant impact in a rapidly evolving industry.