Medicaid Work Requirements in 2025: Impact on Enrollment

Proposed changes to Medicaid work requirements in 2025 are projected to significantly impact enrollment rates by potentially reducing the number of eligible individuals as stricter criteria are implemented, requiring beneficiaries to meet specific work-related activities to maintain their coverage.
The potential changes to Medicaid work requirements are stirring debate, with many questioning how will the proposed changes to Medicaid work requirements affect enrollment rates in 2025?
Understanding Medicaid Work Requirements
Medicaid, as a cornerstone of the US healthcare system, provides crucial medical coverage to millions of low-income Americans. A key aspect of the program is its eligibility criteria, which have evolved over time to include certain work requirements in some states. These requirements, designed to promote self-sufficiency, mandate that beneficiaries engage in specific work-related activities to maintain their coverage. Understanding the framework of these mandates is essential to evaluate how potential alterations may impact enrollment rates.
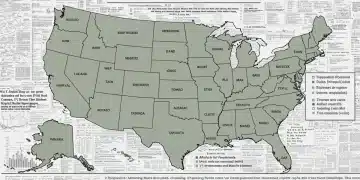
Medicaid work requirements are not uniformly applied across the United States. Instead, they are typically implemented through waivers granted by the Centers for Medicare & Medicaid Services (CMS). These waivers allow states to impose conditions on Medicaid eligibility that go beyond those established in federal law. The purpose behind these work requirements is multifaceted, with proponents arguing that they incentivize employment, reduce dependency on public assistance programs, and encourage healthier lifestyles through work participation.
Historical Context and Evolution
The concept of linking Medicaid eligibility to work-related activities is not new. It has been a topic of discussion and experimentation for decades. However, it gained significant traction under the Trump administration, which encouraged states to seek waivers to implement work requirements. Several states, including Arkansas, Kentucky, and Indiana, adopted such policies, but they faced numerous legal challenges and implementation hurdles.
The Biden administration has since expressed significant reservations about work requirements, leading to the rescission of several approved waivers. This shift in policy reflects concerns about the potential impact on coverage rates and access to care for vulnerable populations.
Current Status of Work Requirements
As of 2024, the status of Medicaid work requirements remains fluid. Some states continue to pursue or maintain their policies, while others have paused or abandoned their efforts. Court decisions and federal policy changes have significantly influenced the landscape, creating an uncertain environment for both beneficiaries and healthcare providers.
- States like Georgia and Utah have either implemented or are in the process of implementing work requirements with varying degrees of enforcement.
- Arkansas’s work requirement faced significant legal challenges and was eventually blocked by the courts.
- The Biden administration has consistently signaled its opposition to strict work requirements, emphasizing the need to prioritize coverage and access to care.
The implications of Medicaid work requirements are broad, affecting not only individuals enrolled in the program but also healthcare providers, state budgets, and the overall healthcare system. As states navigate the legal, political, and practical challenges of implementing these policies, it is crucial to consider the potential effects on enrollment rates and access to essential medical services. This background provides a foundation for understanding the proposed changes and their projected impacts in 2025.
Proposed Changes to Medicaid in 2025
The landscape of Medicaid policies is continuously evolving, with proposed changes often reflecting shifts in political priorities and evolving healthcare needs. As we look ahead to 2025, several key policy modifications are under consideration that could significantly affect Medicaid beneficiaries and enrollment rates. A thorough examination of these proposed changes is essential for understanding their potential implications.
One of the most prominent proposals involves the modification of existing work requirements or the introduction of new ones in several states. These changes aim to mandate that Medicaid beneficiaries engage in a certain number of work hours per week or participate in job training programs to maintain their eligibility.
Specifics of Proposed Work Requirements
The specifics of these proposed work requirements vary by state but generally include provisions such as a minimum number of required work hours, exemptions for specific groups (e.g., pregnant women, individuals with disabilities, and caregivers), and reporting requirements to ensure compliance. Some proposals also include provisions for job training and volunteer activities to count toward the work requirement.
These changes target adults ages 19-64 who are not pregnant or disabled. Exceptions are often included for those in school, those who are primary caregivers, or those who are medically frail.
Eligibility Criteria Modifications
Beyond work requirements, there are also proposals to modify other eligibility criteria for Medicaid. These changes could include adjustments to income thresholds, asset limits, and residency requirements. Some states are considering stricter verification processes to ensure beneficiaries meet these criteria.
- Changes to income thresholds could result in some individuals becoming ineligible for Medicaid due to income exceeding the set limits.
- Stricter asset limits might disqualify individuals who have savings or other assets above the allowable amount.
- Enhanced verification processes could make it more difficult for eligible individuals to enroll or maintain coverage due to administrative burdens.
Potential Challenges and Legal Hurdles
The implementation of these proposed changes is not without challenges. Many of these policies have faced legal scrutiny, with advocacy groups arguing that they violate federal Medicaid law and disproportionately harm vulnerable populations. Legal challenges often focus on whether the changes align with the core objectives of Medicaid and whether they unduly restrict access to healthcare.

By understanding the specifics of these proposed changes, stakeholders can better anticipate their potential impacts and advocate for policies that promote equitable access to healthcare. The upcoming year will be crucial in setting the trajectory for Medicaid and its beneficiaries.
Predicting Enrollment Rate Changes in 2025
Forecasting enrollment rate changes in Medicaid following the implementation of proposed work requirements involves a complex analysis of various factors. Understanding the potential impact requires considering historical data, economic conditions, and the specifics of the new policies.
Historical data from states that have previously implemented work requirements provides valuable insights. For instance, Arkansas’s experience with work requirements led to significant drops in enrollment rates. A 2018 study found that over 17,000 individuals lost coverage within the first few months of implementation. However, the effectiveness of these policies is often debated due to legal challenges and implementation issues.
Economic Factors
Economic conditions play a crucial role in determining Medicaid enrollment rates. During periods of economic expansion, fewer people tend to rely on Medicaid. Conversely, economic downturns often lead to increased enrollment as more individuals lose their jobs and income. The economic outlook for 2025 will, therefore, be a significant factor in predicting enrollment changes.
Demographic Considerations
Different demographic groups are likely to be affected differently by the proposed changes. For example, individuals with disabilities, older adults, and those living in rural areas may face greater challenges in meeting work requirements due to limited job opportunities and transportation barriers.
- Adults without dependent children may find it particularly difficult to meet work requirements due to a lack of support systems.
- Low-income individuals might struggle to balance work and compliance with Medicaid requirements because of the need to switch employers for better working conditions.
- Rural populations may face challenges because of limited job options and access to transportation.
Impact of Stricter Eligibility Criteria
Stricter income verification requirements and asset limits, beyond just work requirements, can directly affect Medicaid enrollment rates. These tougher standards can make it harder for eligible individuals to enroll or stay on the program.
Some people may be discouraged by the complexity of the enrollment process, leading to a reduction in enrollment, even among those who are eligible. Others may struggle to provide all the necessary documentation. Research from states with strict documentary requirements for voting, for example, shows that even eligible citizens may not participate because of documentation hurdles.
The introduction of work requirements and stricter eligibility checks in 2025 is likely to lead to lower Medicaid enrollment. However, the exact scale of this decrease will depend on how well the state enforces these rules and how efficiently it communicates any exceptions to beneficiaries. Continuous monitoring of enrollment data and feedback from beneficiaries will be crucial to addressing unintended consequences and ensuring people have access to the care they need.
Potential Benefits of Work Requirements
While work requirements in Medicaid have sparked considerable debate, they also present potential benefits that are worth considering. Proponents argue they can encourage self-sufficiency, improve health outcomes, and reduce dependence on public assistance.
The primary argument for work requirements is that they can encourage beneficiaries to seek and maintain employment. By incentivizing work, these policies can help individuals gain financial independence and reduce their reliance on government support. This aligns with the broader goal of promoting personal responsibility and self-sufficiency.
Improved Health Outcomes
Participation in the workforce can lead to improved health outcomes for several reasons. Employment often provides access to employer-sponsored health insurance, which can supplement Medicaid coverage. Additionally, work can promote physical activity, social interaction, and a sense of purpose, all of which contribute to better overall well-being.
Reduced Dependence on Public Assistance
Another potential benefit of work requirements is the reduction of long-term dependence on public assistance programs. By helping individuals transition from Medicaid to employer-sponsored insurance, these policies can free up resources to support other vulnerable populations and promote the long-term sustainability of Medicaid.
Increased State Revenue
When more people are employed and earning income, states may see increased tax revenue. This added revenue could be used to fund various state programs, including healthcare initiatives, making the state’s budget less strained overall.
- Work requirements might help Medicaid beneficiaries find jobs and become less dependent on government aid.
- Working can boost physical activity and social connections, which are good for overall health.
- More people working means more state tax revenues, which can fund essential services.
However, it’s vital to weigh these theoretical benefits against the real-world effects, particularly on people who face serious obstacles to employment. When implemented thoughtfully, work requirements can potentially improve individual well-being and the sustainability of public programs.
Negative Impacts of Work Requirements on Enrollment
Although there are potential benefits to Medicaid work requirements, numerous negative impacts on enrollment rates and access to healthcare must be considered. These include reduced coverage, administrative burdens, and disproportionate effects on vulnerable populations.
One of the most significant concerns about work requirements is their potential to reduce Medicaid coverage. Many eligible individuals may struggle to meet the requirements due to various barriers, such as lack of job opportunities, transportation issues, and health limitations. As a result, they may lose their Medicaid coverage, leading to reduced access to essential medical services.
Administrative Burdens
Implementing and enforcing work requirements can impose significant administrative burdens on both beneficiaries and state agencies. Beneficiaries must navigate complex reporting requirements and documentation processes, while state agencies must invest in additional staff and resources to verify compliance. These administrative costs can divert resources away from other essential healthcare services.
Disproportionate Impact on Vulnerable Populations
Work requirements often disproportionately affect vulnerable populations, such as individuals with disabilities, older adults, and those living in rural areas. These groups may face greater challenges in meeting the requirements due to limited job opportunities, transportation barriers, and health limitations.
- Some states may struggle to support beneficiaries in finding suitable jobs or managing compliance, leading to coverage loss.
- Work requirements can make the process more complex, potentially discouraging eligible individuals from enrolling.
- These requirements could lead to poorer health outcomes for those who lose coverage and may increase healthcare costs in the long run.
Therefore, while work requirements may support principles of self-sufficiency, they can also create serious problems for healthcare access and affordability.
Strategies to Mitigate Negative Enrollment Impacts
Given the potential negative impacts of Medicaid work requirements on enrollment rates, it is essential to develop strategies to mitigate these effects. These strategies should focus on ensuring that eligible individuals maintain coverage while promoting self-sufficiency and responsible stewardship of public resources.
One key strategy is to provide comprehensive support services to help Medicaid beneficiaries meet work requirements. These services may include job training, job placement assistance, transportation assistance, and childcare support. By addressing the barriers that individuals face in finding and maintaining employment, these services can help them comply with work requirements and maintain their Medicaid coverage.
Streamlined Enrollment Processes
Streamlining the enrollment process can help reduce administrative burdens and ensure that eligible individuals can easily enroll in Medicaid. This may involve simplifying application forms, reducing documentation requirements, and offering online enrollment options. By making it easier to enroll, states can minimize the number of eligible individuals who lose coverage due to administrative hurdles.
Exemptions and Accommodations
Offering targeted exemptions and accommodations can help protect vulnerable populations from the negative effects of work requirements. This may include exemptions for individuals with disabilities, older adults, pregnant women, and caregivers. Additionally, states can provide accommodations for individuals who face unique challenges in meeting the requirements, such as those living in rural areas with limited job opportunities.
- Providing childcare assistance helps parents work without worrying about their children’s care.
- Allowing people to count job training or volunteer work toward work requirements can make it easier to comply.
- Transportation help can enable people in rural areas to get to work or training programs.
By implementing these strategies, states can mitigate the negative impacts of Medicaid work requirements on enrollment rates and ensure that eligible individuals maintain access to essential healthcare services. Continuous monitoring and evaluation will be essential to assess the effectiveness of these strategies and make adjustments as needed.
| Key Point | Brief Description |
|---|---|
| Changes to Work Mandates | Medicaid recipients have to work a number of hours each month to be eligible. |
| Eligibility Impact | New stricter eligibility rules will likely cause some people to lose or fail to get Medicaid coverage. |
| Vulnerable Access | People with disabilities, older adults, and rural residents may have trouble meeting work needs, affecting coverage. |
| Support Access | Support services like job training are expected to offset these policy effects. |
Frequently Asked Questions
▼
Medicaid work requirements are rules that require certain adults to work, volunteer, or attend job training for a specific number of hours each month to keep their health coverage.
▼
Work requirements primarily affect adults between 19 and 64 who are not pregnant or have a disability. Some people are exempt based on their particular status.
▼
Work requirements can lead to reduced enrollment because some eligible individuals may struggle to meet the requirements due to barriers such as lack of job opportunities or health issues.
▼
Yes, exemptions typically exist for individuals with disabilities, pregnant women, older adults, and primary caregivers of dependent children, because they need additional care.
▼
Support services include job training, job placement assistance, transportation assistance, and childcare to help individuals meet the work requirements and maintain their health coverage.
Conclusion
In summary, the introduction of work requirements and stricter eligibility checks will present challenges to Medicaid enrollment rates. Continuous monitoring of enrollment data and feedback from beneficiaries will be crucial to addressing unintended consequences and ensuring people have access to the care they need.