FDA Approval for MedTech Startups: A Step-by-Step US Guide

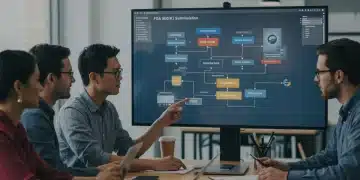
Navigating FDA approval for medtech startups in the US involves a structured process, including understanding regulatory pathways, preparing documentation, undergoing inspections, and ensuring post-market compliance to successfully introduce innovative medical devices to the American market.
Are you a medtech startup aiming to launch your innovative medical device in the US market? Understanding and successfully navigating the FDA approval process is crucial. This step-by-step guide provides essential insights and strategies for medtech startups to achieve FDA clearance or approval.
Understanding the FDA Regulatory Landscape
The Food and Drug Administration (FDA) plays a pivotal role in ensuring the safety and efficacy of medical devices in the United States. For medtech startups, a solid understanding of the FDA’s regulatory framework is the critical first step in bringing their innovations to market.
Navigating this landscape can be complex, and it’s important to understand the different device classifications and regulatory pathways available.
Device Classifications
The FDA classifies medical devices into three categories based on risk:
- Class I: These devices pose the lowest risk and are subject to general controls, such as labeling requirements.
- Class II: These devices pose moderate risk and require special controls, such as performance standards and post-market surveillance. Most medtech startups will fall into this category.
- Class III: These devices pose the highest risk and require premarket approval (PMA), which involves a rigorous review process.
The classification of your device will determine the regulatory pathway you need to follow.
Regulatory Pathways
There are several pathways to market, with the most common being:
- 510(k) Premarket Notification: This pathway is for Class II devices that are substantially equivalent to a predicate device already on the market.
- Premarket Approval (PMA): This pathway is required for Class III devices and involves demonstrating reasonable assurance of safety and effectiveness.
- De Novo Classification: This pathway is for novel devices with low to moderate risk that do not have a predicate device.
Choosing the right pathway is a strategic decision that can impact the time and cost of bringing your device to market.
In summary, understanding the FDA’s regulatory landscape, including device classifications and available pathways, is a fundamental step for medtech startups. This knowledge will guide the entire approval process and ensure a smoother path to market.
Developing a Regulatory Strategy
With a foundational understanding of the FDA’s regulatory landscape, the next essential step for medtech startups is to craft a well-defined regulatory strategy. This involves not only compliance but also strategic planning to optimize the approval process.
A comprehensive regulatory strategy will serve as a roadmap, guiding your team through the necessary steps and helping you make informed decisions along the way.
Identifying the Right Regulatory Pathway
Selecting the most appropriate regulatory pathway is a crucial component of your regulatory strategy. Consider the following factors:
- Device Classification: As discussed earlier, your device’s classification will dictate the available pathways.
- Predicate Device: If your device is similar to a device already on the market, the 510(k) pathway may be a viable option.
- Novelty: If your device is novel and doesn’t have a predicate, the De Novo pathway may be appropriate.
Carefully evaluate these considerations to make an informed decision.
Preparing for FDA Interactions
Engaging with the FDA early in the process can be beneficial. Consider the following types of interactions:
- Pre-Submission Meetings: These meetings allow you to get feedback from the FDA on your proposed regulatory strategy and study design.
- Informational Meetings: Use these meetings to clarify specific regulatory requirements.
Preparing thoroughly for these interactions will help you get the most out of them.

Developing a robust regulatory strategy requires careful analysis and proactive planning. By identifying the right pathway and preparing for FDA interactions, medtech startups can streamline the approval process and increase their chances of success.
Preparing the 510(k) Submission
For many medtech startups, the 510(k) pathway represents the most efficient route to market for Class II devices. Successfully preparing a 510(k) submission involves meticulous documentation and a clear demonstration of substantial equivalence to a predicate device.
A well-prepared 510(k) submission can significantly reduce review times and increase your chances of clearance.
Essential Elements of a 510(k) Submission
A 510(k) submission must include the following elements:
- Device Description: A detailed description of your device, including its intended use and operating principles.
- Predicate Device Information: Information on the predicate device, including its 510(k) number and any relevant performance data.
- Performance Data: Data demonstrating that your device is as safe and effective as the predicate device. This may include bench testing, animal studies, or clinical trials.
Ensure that all information is accurate and well-organized.
Demonstrating Substantial Equivalence
The key to a successful 510(k) submission is demonstrating that your device is substantially equivalent to the predicate device. This means showing that your device has:
- The same intended use as the predicate device.
- The same technological characteristics as the predicate device, or if there are differences, that the differences do not raise new questions of safety and effectiveness.
Provide detailed data and analysis to support your claims of substantial equivalence.
In conclusion, preparing a comprehensive and well-documented 510(k) submission is crucial for medtech startups seeking FDA clearance. By including all essential elements and thoroughly demonstrating substantial equivalence, you can increase your chances of a successful outcome.
Navigating the Premarket Approval (PMA) Process
For Class III medical devices, which pose the highest risk, the Premarket Approval (PMA) process is the required pathway to market. This process is more rigorous and demanding compared to the 510(k) pathway, requiring extensive data and analysis to demonstrate the safety and effectiveness of the device.
Successfully navigating the PMA process requires a deep understanding of FDA requirements and a commitment to thorough scientific investigation.
Key Components of a PMA Application
A PMA application is a comprehensive document that includes:
- Full Reports of All Studies: Detailed reports of all preclinical and clinical studies conducted to evaluate the safety and effectiveness of the device.
- Manufacturing Information: Detailed information about the manufacturing process, including quality control procedures.
- Proposed Labeling: The proposed labeling for the device, including instructions for use and any warnings or precautions.
Each component must be thoroughly documented and supported by scientific evidence.
Clinical Trials for PMA Approval
Clinical trials are a critical aspect of the PMA process. These trials are designed to evaluate the safety and effectiveness of the device in a real-world setting.
- Study Design: The study design must be rigorous and statistically sound.
- Data Collection: Data must be collected accurately and consistently.
- Analysis: The data must be analyzed using appropriate statistical methods.
The results of the clinical trials must demonstrate that the device is safe and effective for its intended use.
In summary, the PMA process is a complex and demanding pathway to market for Class III medical devices. By understanding the key components of a PMA application and conducting rigorous clinical trials, medtech startups can increase their chances of obtaining FDA approval.
Manufacturing and Quality System Compliance
Beyond the scientific and clinical aspects of FDA approval, medtech startups must also focus on manufacturing and quality system compliance. The FDA’s Quality System Regulation (QSR) outlines the requirements for manufacturing medical devices in a consistent and reliable manner.
Compliance with the QSR is essential for ensuring the safety and effectiveness of your devices and avoiding potential regulatory issues.
Understanding the Quality System Regulation (QSR)
The QSR covers various aspects of the manufacturing process, including:
- Design Controls: Procedures for designing and developing medical devices.
- Production and Process Controls: Procedures for manufacturing and controlling the production process.
- Corrective and Preventive Actions (CAPA): Procedures for identifying and correcting quality issues.
Implementing a robust quality system is crucial for compliance.
Preparing for FDA Inspections
The FDA conducts inspections of manufacturing facilities to ensure compliance with the QSR. Preparing for these inspections involves:
Ensuring that all processes and procedures are documented and followed.
Training all employees on the requirements of the QSR.
Conducting internal audits to identify and correct any deficiencies.

In conclusion, manufacturing and quality system compliance are critical components of the FDA approval process for medtech startups. By understanding the QSR and preparing for FDA inspections, you can ensure that your devices are manufactured to the highest standards of quality and safety.
Post-Market Surveillance and Compliance
The journey to FDA approval doesn’t end once your device is on the market. Post-market surveillance and compliance are essential for ensuring the continued safety and effectiveness of your product and meeting ongoing regulatory requirements.
A proactive approach to post-market surveillance can help you identify and address any potential issues before they escalate.
Reporting Adverse Events
Medtech startups are required to report adverse events associated with their devices to the FDA. This includes:
- Device Malfunctions: Any malfunction of the device that could lead to serious adverse health consequences.
- Serious Injuries: Any serious injury associated with the use of the device.
- Deaths: Any death associated with the use of the device.
Timely and accurate reporting is crucial for maintaining compliance.
Post-Market Studies
In some cases, the FDA may require medtech startups to conduct post-market studies to further evaluate the safety and effectiveness of their devices. These studies may be required if there are concerns about the long-term performance of the device or if there are specific questions that need to be addressed.
In summary, post-market surveillance and compliance are essential for ensuring the continued safety and effectiveness of medical devices. By reporting adverse events and conducting post-market studies, medtech startups can meet their ongoing regulatory obligations and protect patient safety.
| Key Aspect | Brief Description |
|---|---|
| 💡 Regulatory Strategy | Choosing the right pathway and preparing for FDA interactions. |
| 🔬 510(k) Submission | Demonstrating substantial equivalence to a predicate device. |
| 🏭 Manufacturing Compliance | Adhering to the FDA’s Quality System Regulation (QSR). |
| 📊 Post-Market Surveillance | Reporting adverse events and conducting post-market studies. |
FAQ
▼
The first step is to determine the correct classification and regulatory pathway for your medical device by engaging with the FDA.
▼
The 510(k) process demonstrates substantial equivalence to existing devices, while PMA requires proof of safety and effectiveness.
▼
A predicate device is a legally marketed device to which your device’s substantial equivalence can be compared.
▼
Quality system compliance ensures that your device is manufactured consistently and safely, meeting FDA’s standards.
▼
Post-market surveillance involves monitoring your device’s performance in the market and reporting any adverse events to the FDA.
Conclusion
Navigating the FDA approval process for medtech startups in the US is a challenging yet essential endeavor. By understanding the regulatory landscape, developing a robust strategy, and focusing on compliance, startups can successfully bring their innovative medical devices to market and improve patient outcomes.