AI Telehealth Expands Specialist Access to 3M Rural US Patients

AI-enhanced telehealth bridges the specialist access gap for 3 million rural US patients by leveraging artificial intelligence to improve diagnostics, personalize treatments, and streamline healthcare delivery, fostering healthier communities.
Imagine a future where specialist healthcare is readily available, regardless of geographical limitations. AI-enhanced telehealth is making this vision a reality, significantly expanding access to specialist care for 3 million rural US patients, and potentially many more.
The Urgent Need for Specialist Access in Rural America
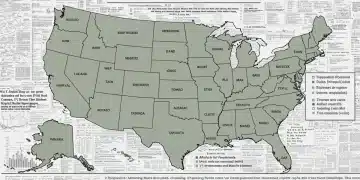
Rural communities across the United States face significant challenges in accessing specialist healthcare. Geographic isolation, limited transportation options, and a shortage of healthcare professionals all contribute to this disparity. This lack of access often leads to delayed diagnoses, inadequate treatment, and poorer health outcomes for rural residents.
The Impact of Geographical Barriers on Healthcare Access
Geographical barriers are a primary obstacle to specialist care in rural areas. The distance to the nearest specialist can be prohibitive, especially for individuals with mobility issues or limited financial resources. This problem is exacerbated by the fact that many rural communities lack public transportation options, making it difficult for residents to travel to urban centers for medical appointments.
Specialist Shortages in Rural Communities
Many rural areas struggle with a shortage of specialist physicians, which means that rural residents often have to wait longer for appointments, travel long distances to see a specialist, or simply forgo specialist care altogether. This is where AI-enhanced telehealth can step in to fill gaps.
- Telehealth provides convenient access to specialist care from the comfort of home.
- AI algorithms can support healthcare providers in making more accurate diagnoses.
- Remote patient monitoring can help specialists track patient progress, leading to more personalized treatments.

In conclusion, the need for specialist access in rural America is critical. Geographical barriers and specialist shortages contribute to poorer health outcomes for rural residents. AI-enhanced telehealth offers a promising solution to these challenges, bridging the gap between rural patients and specialist care.
How AI is Transforming Telehealth for Rural Patients
AI is revolutionizing telehealth by enhancing its capabilities and improving the quality of care delivered to rural patients. From AI-powered diagnostic tools to personalized treatment plans, AI is making telehealth more effective, efficient, and accessible than ever before. These tools not only enhance the existing telehealth infrastructure but also promise to extend its reach to even more remote areas.
AI-Powered Diagnostic Tools
AI-powered diagnostic tools enable healthcare providers to remotely assess and diagnose patients with greater accuracy and efficiency. These tools can analyze medical images, patient data, and other relevant information to help providers identify potential health problems and make informed treatment decisions. This is particularly useful in fields like radiology and cardiology where immediate and accurate diagnoses are crucial.
Personalized Treatment Plans
AI algorithms are capable of analyzing vast amounts of patient data to develop personalized treatment plans tailored to individual needs. By considering factors such as medical history, lifestyle, and genetic information, AI can help providers create treatment plans that are more effective and less likely to cause adverse reactions. This level of personalization is especially valuable in managing chronic conditions, ensuring patients receive the most appropriate care.
Beyond diagnostics and personalized treatment plans, AI contributes significantly to telehealth through:
- Automated administrative tasks that streamline workflows for healthcare providers.
- Predictive analytics that identify patients at risk of developing certain conditions or experiencing health crises.
- Natural language processing that improves communication between patients and providers.
In conclusion, AI is transforming telehealth by enhancing its capabilities, improving the quality of care delivered to rural patients, and making it more accessible than ever. From diagnostic tools to personalized treatment plans, AI is playing a key role in revolutionizing telehealth for rural populations.
Real-World Examples of AI-Enhanced Telehealth Success
The transformative potential of AI-enhanced telehealth is not just theoretical; it is being realized in real-world settings across the United States. Several healthcare organizations and telehealth providers have successfully implemented AI-powered solutions to improve specialist access for rural patients, resulting in tangible benefits for both patients and providers. These examples highlight the versatility and effectiveness of integrating AI into telehealth practices.
Case Study 1: Improved Stroke Care in Rural Hospitals
A rural hospital implemented an AI-powered telemedicine platform that allows stroke specialists to remotely assess patients and make treatment recommendations. The AI algorithms analyze brain scans and other medical data to help specialists quickly determine the best course of action. This has significantly reduced the time it takes for rural patients to receive life-saving stroke treatment, improving their chances of recovery.
Case Study 2: Enhanced Diabetes Management in Underserved Communities
A telehealth provider partnered with a community health center to offer AI-driven diabetes management services to patients in underserved communities. The AI algorithms monitor patient blood sugar levels, medication adherence, and lifestyle habits to provide personalized guidance and support. This has led to improved blood sugar control, reduced hospitalizations, and better overall health outcomes for patients with diabetes.

The success of AI- enhanced telehealth is evident through:
- Reduced wait times for specialist appointments, enabling timely access to care.
- Improved patient engagement, as AI facilitates personalized education and support.
- Cost savings for patients and healthcare providers, due to reduced travel expenses and hospital readmissions.
In conclusion, real-world examples demonstrate that AI-enhanced telehealth is a successful approach to improving specialist access for rural patients. These case studies highlight the tangible benefits of AI in telehealth, including improved stroke care, enhanced diabetes management, and better overall health outcomes for rural residents.
Overcoming Challenges in Implementing AI-Enhanced Telehealth
While AI-enhanced telehealth holds immense promise for improving specialist access in rural areas, implementing these systems requires careful consideration of several challenges. Addressing these challenges proactively is crucial to ensure the successful and sustainable deployment of AI-powered telehealth solutions in rural healthcare settings. These include data privacy and security concerns, the digital divide, and the need for additional training and support.
Data Privacy and Security Concerns
Data privacy and security are primary concerns when implementing AI-enhanced telehealth systems. The collection, storage, and transmission of sensitive patient data must be protected to prevent unauthorized access and data breaches. Compliance with regulations such as HIPAA is essential to maintain patient trust and safeguard their privacy rights.
Addressing the Digital Divide
The digital divide, or the gap between those who have access to technology and those who do not, poses a significant barrier to the widespread adoption of AI-enhanced telehealth in rural areas. Many rural communities lack access to reliable broadband internet, which is necessary for telehealth services. This digital divide can exacerbate existing healthcare disparities, making it even more difficult for rural residents to access specialist care.
There are, however, many solutions to overcome such challenges:
- Investing in broadband infrastructure to improve internet connectivity in rural areas.
- Developing culturally appropriate telehealth solutions that meet the unique needs of rural communities.
- Providing technical assistance and support to rural healthcare providers to help them implement and use AI-enhanced telehealth systems effectively.
In conclusion, overcoming the challenges in implementing AI-enhanced telehealth requires a multifaceted approach that addresses data privacy concerns, bridges the digital divide, and provides adequate training and support. By proactively addressing these challenges, healthcare providers and policymakers can ensure that AI-enhanced telehealth reaches its full potential in improving specialist access for rural patients.
The Future of AI and Telehealth: Predictions and Possibilities
The convergence of AI and telehealth is still in its early stages, but the future holds tremendous potential for further innovation and expansion. As AI technology continues to evolve, it is likely to play an even greater role in transforming telehealth and improving access to healthcare for rural populations. Expect to see a growing emphasis on remote patient monitoring and the use of wearables to collect real-time health data.
Increased Focus on Remote Patient Monitoring
Remote patient monitoring (RPM) technologies are already being used to track patient vital signs, medication adherence, and other health indicators from afar. With the help of AI, RPM data can be analyzed in real-time to identify potential health problems and provide timely interventions. This is particularly valuable for managing chronic conditions.
Wearable Technology Integration
Wearable technology, such as smartwatches and fitness trackers, is becoming increasingly sophisticated and capable of collecting a wide range of health data. This data can be integrated into AI-enhanced telehealth systems to provide a more comprehensive picture of a patient’s health status. AI algorithms can then use this information to personalize treatment plans and provide tailored recommendations.
In tandem with wearables and RPM, here are some additional future possibilities:
- Advancements in AI-powered virtual assistants that can answer patient questions, schedule appointments, and provide basic medical advice.
- The development of AI algorithms that can predict and prevent disease outbreaks in rural communities.
- Greater collaboration between healthcare providers, technology companies, and policymakers to drive innovation and improve access to care.
In conclusion, the future of AI and telehealth is bright, with tremendous potential for further innovation and expansion. By embracing remote patient monitoring, integrating wearable technology, and fostering collaboration, healthcare stakeholders can unlock the full potential of AI-enhanced telehealth to improve specialist access and enhance the health and well-being of rural communities.
Policy and Funding: Supporting AI-Enhanced Telehealth Initiatives
The successful implementation and widespread adoption of AI-enhanced telehealth require supportive policies and adequate funding. Policymakers and healthcare organizations must work together to create an environment that encourages innovation, promotes telehealth adoption, and ensures that rural communities have access to the resources they need to benefit from these technologies. Changes in regulations surrounding telehealth are paving the way for more widespread adoption.
Regulatory Changes and Reimbursement Policies
Regulatory changes, such as those related to telehealth licensure and reimbursement policies, can have a significant impact on the adoption of AI-enhanced telehealth. Policymakers should consider implementing policies that make it easier for healthcare providers to offer telehealth services across state lines and ensure that providers are adequately reimbursed for the telehealth services they provide. Expansion of coverage from insurers can significantly shift the landscape for telehealth applications.
Federal and State Funding Opportunities
Federal and state funding opportunities can provide crucial financial support for AI-enhanced telehealth initiatives. These funding opportunities can be used to support telehealth infrastructure development, provider training, and the implementation of AI-powered solutions. Targeted funding can help to encourage innovation particularly in underserved areas.
Government and other organizations can support development through:
- Incentivizing private investments in telehealth infrastructure and technology development.
- Promoting public-private partnerships to accelerate the adoption of AI-enhanced telehealth.
- Measuring the impact of AI-enhanced telehealth on healthcare access, quality, and costs to inform future policy decisions.
In conclusion, supportive policies and adequate funding are essential for the successful implementation and widespread adoption of AI-enhanced telehealth. By addressing regulatory barriers, investing in telehealth infrastructure, and incentivizing innovation, policymakers can help ensure that AI-enhanced telehealth reaches its full potential in improving specialist access for rural patients.
| Key Point | Brief Description |
|---|---|
| 📍Rural Access | AI Telehealth expands specialist care to 3M rural US patients. |
| 🤖 AI Transformation | AI enhances diagnostics, personalization, and efficiency in rural telehealth. |
| ✔️ Real Success | Case studies show improved stroke/diabetes care via AI Telehealth. |
| 🛡️Policy Support | Supportive policy and funding are vital for AI Telehealth success. |
Frequently Asked Questions
▼
AI enhances telehealth through better diagnostics, personalized treatment plans, predictive analytics, and automating administrative tasks, making healthcare more efficient and accessible.
▼
Challenges include data privacy concerns, the digital divide (lack of internet access), and the need for proper training for healthcare providers to use these systems effectively.
▼
RPM involves using technology to track patients’ health data remotely. AI analyzes this data in real-time to identify potential health problems, enabling timely interventions and personalized support.
▼
Governments can help by creating supportive regulatory frameworks, providing funding opportunities for infrastructure, and incentivizing collaboration between healthcare providers and tech companies.
▼
Future advancements include more sophisticated AI-powered virtual assistants, further integration of wearable technology, and AI algorithms for predicting and potentially preventing disease outbreaks.
Conclusion
AI-enhanced telehealth offers a transformative solution to the challenges of specialist access in rural America, promising to bridge geographical gaps, improve health outcomes, and revolutionize healthcare delivery for millions. To fully realize this potential, it is essential to address challenges related to data privacy, digital equity, and workforce training, while also fostering supportive policies and strategic funding initiatives.